Patellar Instability
What is patellar instability?
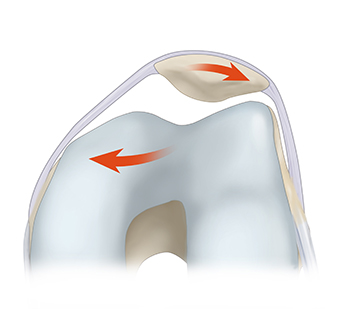
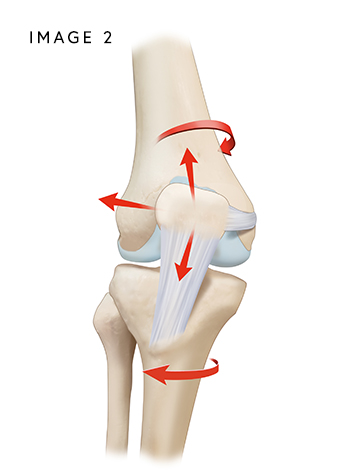
The patella (kneecap) fits in a groove at the end of the femur (thigh bone) and slides up and down, allowing the knee to bend and straighten. There are several ligaments and structures that help maintain the proper alignment and tracking of the patella during these movements.
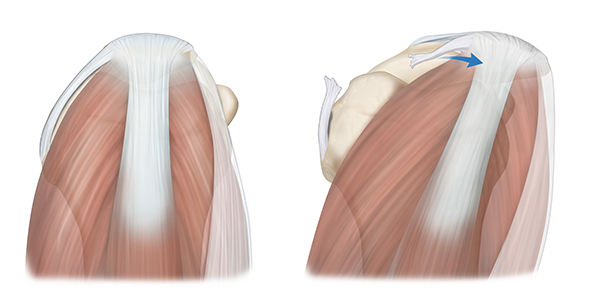
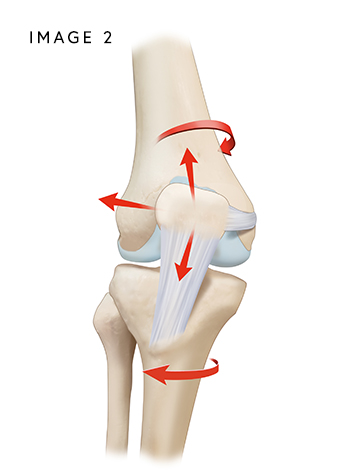
The primary stabilizer of the kneecap is the medial patellofemoral ligament (MPFL). The MPFL connects the medial (inner) edge of the patella to the medial femoral condyle, which is a bony prominence on the medial side of the distal end of the femur. The MPFL helps to stabilize the patella in its groove (trochlea). The lateral patellofemoral ligament (LPFL) attaches to the lateral (outer) edge of the patella and extends to the lateral femoral condyle. Its primary function is to prevent excessive lateral (outward) displacement or dislocation of the patella. The quadriceps tendon connects the quadriceps muscle to the patella and the patellar tendon connects the patella to the shin bone (tibia) below the knee.
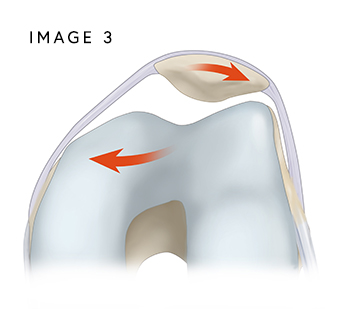
Sometimes, the kneecap can be unstable and dislocate, or slip, out of the trochlea. This causes pain, swelling, stiffness, and persistent joint instability. When the patella slips out of it the trochlea, it is called “patellofemoral instability”, or PFI.
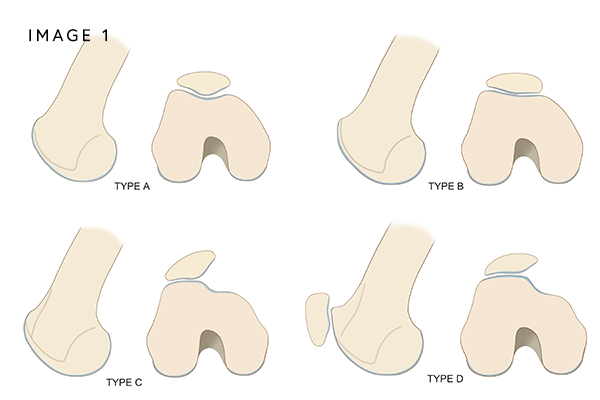
Acute kneecap dislocation and patellar instability is frequently the result of a sports injury, a fall, or a direct impact to the joint that forces the patella out of its normal “track.” Frequently, this is the result of an underlying preexisting condition such as an abnormally high kneecap (patella alta), a shallow groove (trochlear dyplasia), or misalignment of the kneecap and tibia (increased q angle, rotational deformities, etc.), among other abnormalities.
Women and girls have naturally loose ligaments, which predisposes them to lateral patellar dislocation, a common injury in young, active girls and women. Lateral patellar dislocations are the most common knee dislocation injury among young adults, leading to an injury to the MPFL.
The risk of a second dislocation is high after an initial injury, dislocation, or subluxation (partial dislocation) of the patella. Approximately, 15 to 44% of patients who suffer a traumatic dislocation will have recurrent dislocations. Two or more dislocations increase the recurrence rate to over 50%.
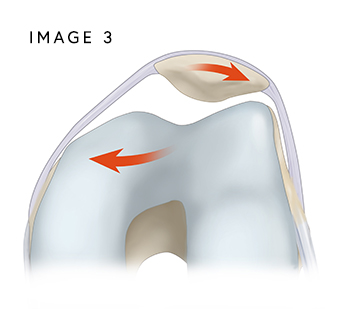
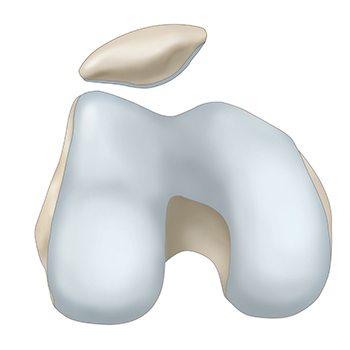
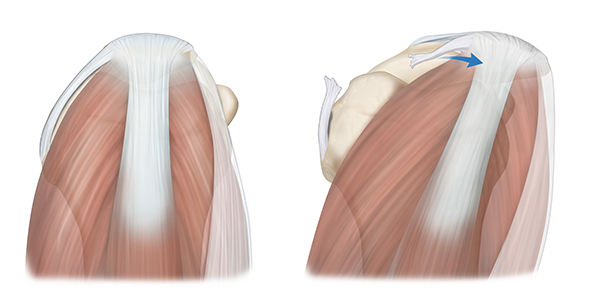
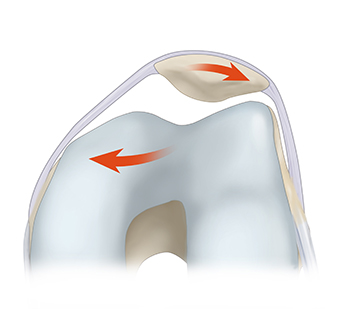
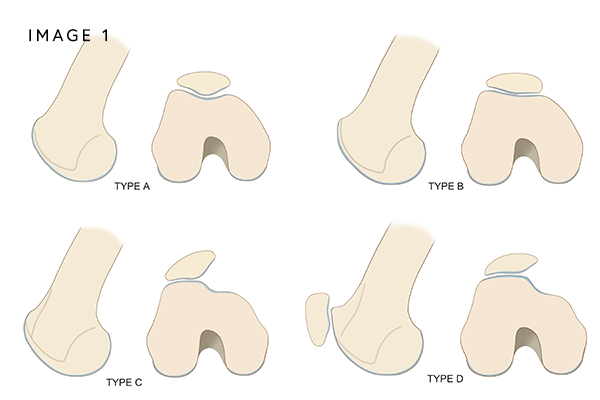
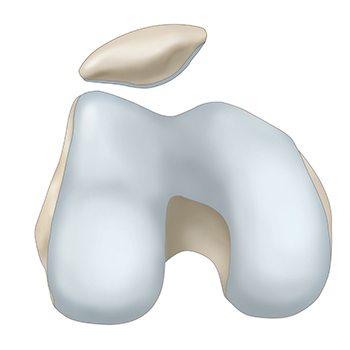
Repeated dislocations are not the result of trauma. Instead, they are caused by a shallow groove (trochlear dysplasia) (Image 1) a kneecap that sits too high (patella alta) (Image 2), bone abnormalities (Image 3), lax muscles (Image 4), ligament injuries including a torn or stretched MPFL, weak quadriceps muscles, and tight hip flexors. Additional risk factors for recurrent instability include young age and sports-related injuries.

Chronic patellar instability is very painful and can significantly limit participation in physical activities due to fear of recurrent dislocations. People who have kneecap instability typically have symptoms that include:
- Swelling and bruising
- Pain while sitting and standing up.
- Pain in the front of the knee
- Joint stiffness
- Knee buckling and catching.
- A creaking sound with knee motion
- Difficulty walking
A combination of a comprehensive history of prior patellar instability episodes, physical examination, x-rays, and an MRI or CT are used to help diagnosis patellar instability. Dr. Jorge Chahla and his team will perform a physical exam that will include observing how the kneecap moves through a range of motion. An X-ray will be obtained to further assess for bony abnormalities predisposing you to patellar instability, including patella alta. An MRI will be ordered to evaluate for soft tissue damage, including a torn MPFL or LPFL. The MRI will also identify any loose bodies within the joint or bone bruising that has resulted from contact between the edge of the knee cap (patellar facet) and the side of the thigh bone (femoral condyle) during a patellar instability episode. Sometimes a CT scan can be used to determine if the bones are not aligned properly.
Patellar instability occurs when the kneecap moves out of its normal position, often leading to dislocations, pain, and difficulty with movement. If left untreated, it can contribute to cartilage damage and long-term knee dysfunction. Dr. Jorge Chahla specializes in diagnosing and treating patellar instability, offering both non-surgical and surgical options to restore knee stability. If you are experiencing recurrent patellar dislocations or knee instability, contact Dr. Chahla’s office in Chicago, Naperville, or Oak Brook for a comprehensive evaluation.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 800 surgeries per year
- Associate professor of orthopedic surgery at Rush University
- Learn more