Shoulder Osteoarthritis
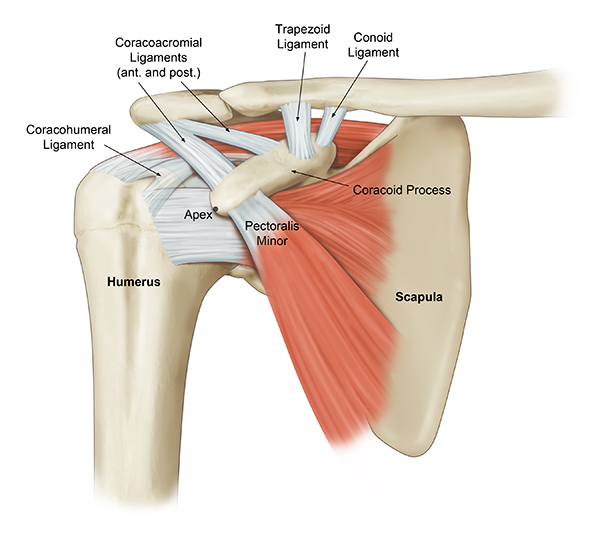
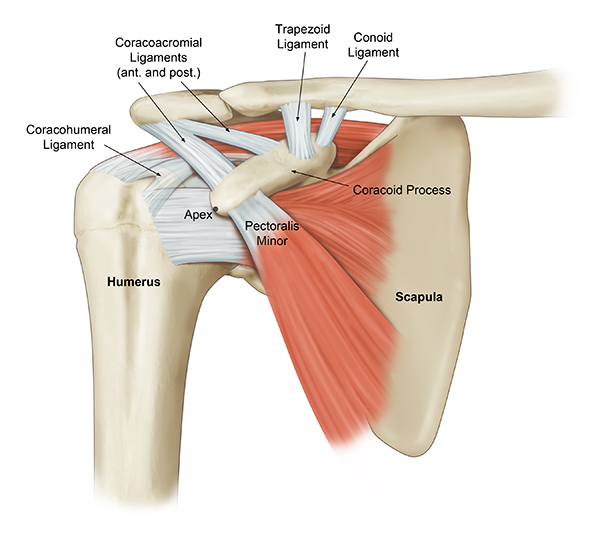
The shoulder is made up of two joints, the acromioclavicular joint and the glenohumeral joint. The glenohumeral joint is a ball and socket joint. The socket is the flat, shallow surface called the glenoid, and the head of the humerus is the ball. Articular cartilage, which is a shiny white tissue, covers both the ball and the socket and functions to reduce friction for smooth joint movement.
Cartilage is the protective tissue that covers the ends of bones in a joint, allowing for smooth and pain-free movement. In shoulder osteoarthritis, the cartilage of the glenoid and humeral head gradually breaks down and wears away, leading to pain, swelling, and difficulty with shoulder movement.
The exact cause of shoulder osteoarthritis can vary, but it is often associated with factors like aging, genetics, previous joint injuries or pathology, and chronic overuse of the shoulder joint.
- Joint Pain: Shoulder osteoarthritis typically causes pain in the shoulder joint. The pain can range from mild to severe. It often worsens with overhead activity, carrying weighted objects, and sleeping.
- Stiffness: People with shoulder OA may experience stiffness in the shoulder joint, making it difficult to move the shoulder through its full range of motion.
- Reduced Range of Motion: As the condition progresses, the range of motion in the shoulder joint may become limited, making it challenging to perform activities like showering, dressing, lifting or pushing objects, and sleeping.
- Crepitus: Some people with shoulder OA may notice a grinding or grating sensation in the shoulder joint, which is known as crepitus.
- Decreased Function: Shoulder osteoarthritis can affect a person’s ability to perform daily activities and participate in physical activities.
- Muscle Weakness: The muscles around the shoulder joint may become weakened due to pain and reduced activity.
- Bone Spurs: Over time, the body may respond to the damage in the joint by forming bony growths or bone spurs at the edges of the joint.
The combination of a detailed history, comprehensive physical examination, and x-rays is the key to a successful diagnosis of shoulder osteoarthritis.
Physical Exam
Dr. Chahla and his team will perform a comprehensive physical exam to assess the range of motion in your shoulder joint, look for signs of inflammation or swelling, and feel for areas of tenderness or crepitus (grating or grinding sensations). The strength of the shoulder will also be evaluated.
Imaging
Diagnostic imaging is necessary to definitively diagnose shoulder osteoarthritis. X-rays will reveal joint space narrowing, the presence of bone spurs, and the extent of cartilage damage.
Shoulder osteoarthritis is a degenerative condition that occurs when the cartilage in the shoulder joint wears down over time, leading to pain, stiffness, swelling, and reduced mobility. This condition can develop due to aging, previous shoulder injuries, or repetitive overhead activities. As the cartilage deteriorates, bone-on-bone friction can cause increased discomfort and limit daily activities. Dr. Jorge Chahla, a leading orthopedic shoulder surgeon, specializes in diagnosing and treating shoulder osteoarthritis, offering both non-surgical and surgical options to relieve pain and restore joint function. If you are experiencing chronic shoulder pain and stiffness, schedule an appointment with Dr. Chahla in Chicago, Naperville, or Oak Brook for expert evaluation and care.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 800 surgeries per year
- Associate professor of orthopedic surgery at Rush University
- Learn more