Cartilage Treatment
What is hip cartilage damage?
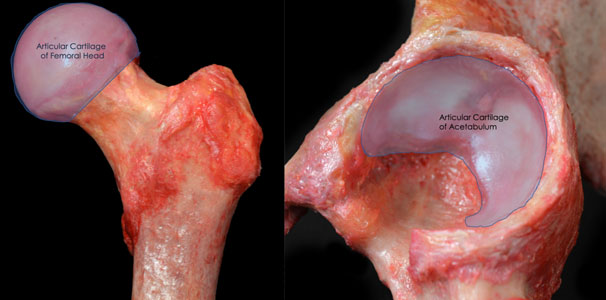
Cartilage is a tough, flexible connective tissue responsible for a variety of different functions in the body. Articular cartilage is complex tissue without any blood supply that consists of cells (chondrocytes) suspended in a collagen matrix. It appears as smooth, white, shiny tissue that covers the surfaces of a joint. The purpose of articular cartilage is to reduce the friction between two bones as they glide over each other within a joint. It also acts as a shock absorber to enable the joint to withstand weight bearing.
Cartilage lesions to the articular cartilage of the hip are common. They can be caused by any trauma such as sudden direct impact, fracture, or fall. Alternatively, degenerative changes from daily wear and tear can lead to cartilage damage. Articular cartilage has no blood supply, so the capacity to repair and heal injured lesions is limited. If left untreated, these lesions can progress to hip arthritis over time. Oftentimes, cartilage lesions of the hip also cause pain and impaired function. As a result, several surgical methods have been developed to restore articular cartilage and help prevent progression to arthritis.
What is microfracture of the hip?
Microfracture is a procedure used to stimulate cartilage regeneration at the area of injury. Multiple, tiny holes are created in the bone beneath the injured cartilage to bring blood and stem cells from the more vascular bone to the surface of the cartilage. This creates an optimal environment for the body to regenerate new cartilage at the injured site.
Who is a good candidate for microfracture treatment of the hip?
Microfracture of the hip is best for patients whose cartilage degeneration is limited to small areas within the hip joint, younger active patients who wish to return to sport or activity, and those who are experiencing significant pain from injured cartilage.
It is not recommended in patients that have widespread arthritis of the hip, those who are inactive, or those who are unwilling to participate in the rehabilitation regimen postoperatively.
What does the procedure entail?
Microfracture of the hip may be performed arthroscopically. This is a minimally invasive procedure that utilizes small incisions with thin instruments and a small camera to see inside the joint. The camera displays the image of the joint on a monitor in the operating room. Sterile fluid is pumped into the hip to expand the joint space and provide room for the surgeon to work.
The area of cartilage damage is prepared by shaving off any frayed cartilage tissue. A sharp tool called an awl is then used to create multiple tiny holes into the bone beneath the cartilage. This stimulates bleeding and allows the cell-rich blood to migrate into the area of cartilage damage, which creates a nourishing environment for cartilage growth.
Oftentimes, orthobiologics are also injected into the hip joint during the time of surgery. Orthobiologics are natural substances such as cells, tissue, blood components, and growth factors that help increase the healing capacity of cartilage. There are a variety of orthobiologics to choose from, including platelet-rich plasma (PRP) or bone marrow aspirate concentrate (BMAC). During surgery, BMAC is obtained from an area of your pelvic bone known as the iliac crest with a specialized syringe. The bone marrow is then spun in a machine for 10-15 minutes to concentrate specialized cells that produce proteins and growth factors for healing. The sample of cells is injected into the joint after microfracturing to help facilitate healing and new cartilage growth.

This procedure is performed in an outpatient surgery center. This means the patient will go home the same day of surgery once they have recovered from anesthesia. At home, patients will be instructed to use crutches for the first few days postoperatively and avoid weight bearing. Most patients will be able to return to sport or other intense activities approximately 4 months after surgery.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 500 surgeries per year
- Assistant professor of orthopedic surgery at Rush University
- Learn more


