Meniscus Repair
What is meniscal repair?
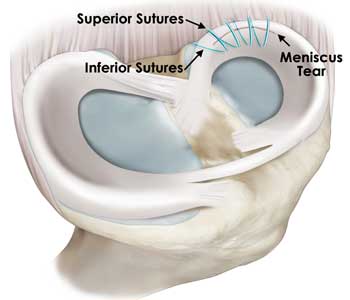
For most patients with acute traumatic meniscus tears, the best treatment modality is a meniscal repair when indicated. The goal of arthroscopic meniscal repair is to use a minimally invasive surgical technique to bring the torn ends of the meniscus together. These ends are then sutured (stitched) together in an attempt to facilitate healing and restoration of a patient’s natural meniscal contour, shape, and function. This will allow for maximal preservation of a patient’s healthy meniscal tissue and minimize long term damage to the cartilage of the knee.
What factors determine if a meniscal repair will be successful?
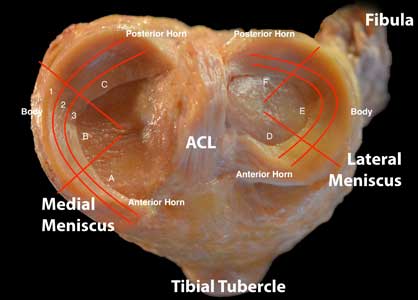
Meniscal repairs tend to heal well when the tear occurs in the peripheral regions of the meniscus (zones 1 and 2 of Figure 1). This is due to the higher blood supply, and thus, healing potential, of the peripheral meniscus. Classically, it has been thought that tears in the central regions of the meniscus do poorly with meniscal repair due to their limited healing ability. While this is true, there is evidence to suggest that meniscal repair can be successful in the more central meniscal regions with less healing potential (zone 3 of Figure 1). Other reasons that one may pursue a meniscal repair include other typical factors including a patient’s age, general health, BMI, and willingness to comply with a postoperative rehabilitation regimen. More recent evidence suggests that patients in their 50s and patients with a BMI below 35 can successfully undergo meniscal repair.
What are the surgical steps of a meniscal repair?
There are several techniques used for meniscal repair. Like, meniscectomies, the procedure is a minimally invasive arthroscopic surgery that uses small incisions to insert an arthroscope (camera) and arthroscopic tools into a patient’s knee joint. Several techniques that are used to bring the meniscal ends together include the inside-out technique, the all-inside technique, and the outside-in technique. Each technique has its own respective strengths and weaknesses based on a meniscal tear size/location, and they can be used in combination with each other for larger tears. During the procedure, Dr. Chahla will use the most optimal combination of techniques to achieve the repair that best restores a patient’s native meniscus structure and function.
What is the postoperative rehabilitation like?
Like all orthopaedic procedures, commitment to a structured post-operative rehabilitation regimen is critical for a satisfactory patient outcome. However, unlike meniscectomies, the rehabilitation protocol for meniscal repair is much more conservative. This is to maximize stability of the repair and minimize damage to the sutured meniscal edges. Failure to adhere to this protocol could result in failure of the repair.
Patients will remain toe-touch weight bearing and use crutches for the first 2 weeks. They will be given a knee brace that they should use for the first 8 weeks after surgery. Without any weight on their leg, patients are allowed to have an active and passive ROM from 0-90 degrees for the first 2 weeks and progress to a full ROM by 4 weeks. After 4 weeks, they can begin weight bearing as tolerated with their knee brace unlocked and will not need their brace after 8 weeks. Patients are expected to begin jogging by approximately 12 weeks and can continue gradually ramping up exercise capacity as tolerated.
When discussing meniscal repair with Dr. Chahla, it is important to consider what your specific goals from the surgery are. Understanding a patient’s goals, activity level, and overall health along with their tear characteristics can help us create the best treatment options for any given patient. Meniscus repair is a suitable option for many patients. For many other patients, meniscus repair is not the best choice. Additionally, understanding the rehabilitation commitment for meniscus repair is critical in determining what the best option is for each patient.
Dr. Chahla and his team of therapists work to provide a supportive social environment and a well-structured recovery plan with clear expectations. This allows patients to flourish and reach their maximal athletic potential.
Dr. Chahla is a nationally renowned, award-winning, fellowship-trained, and board-certified orthopedic sports medicine surgeon. Dr. Chahla has orthopedic clinics in Chicago, Naperville, Oak Brook, and Munster Indiana.
At a Glance
Dr. Jorge Chahla
- Triple fellowship-trained sports medicine surgeon
- Performs over 500 surgeries per year
- Assistant professor of orthopedic surgery at Rush University
- Learn more


